Bariatric Weight-Loss Surgery and Mortality

Today, death rates after weight loss surgery are considered “very low,” occurring in perhaps 1 in 300 to 1 in 500 patients on average.
Obesity treatment has long been tainted by the snake oil scam of profiteers, quacks and quack doctors. Even the modern field of bariatric medicine (derived from the Greek word barosmeaning “weight”) is full of “subtle imagery of sliding.” Lured by the hype of magic pills for quick, useless weight loss, people regret their failure to produce a miracle or see themselves as physically broken. On the other side of the psychological spectrum are overly pessimistic people who hold the view that “fat people are born fat, and there’s not much that can be done about it.” The truth lies somewhere in between.
The difficulty of treating obesity has been compared to learning another language. It’s a success that almost anyone can achieve by investing enough energy, “but it always takes a lot of time and trouble.” And, for those who stick with it, most will regain the lost weight. To me, this speaks of difficulty, rather than vanity. It may take smokers an average of 30 attempts to finally kick the habit. Like quitting smoking, treating obesity is just something that needs to be done. As the chairman of the Association for the Study of Obesity put it, it does not take “will power” to do important tasks such as waking up at night to feed a child; it’s just something that needs to be done.
Our collective response doesn’t seem like rhetoric or reality. If obesity is a “national crisis” of alarming proportions, called by the post-9/11 Surgeon General “everything as bad as terrorism,” why has our reaction been so bitter? For example, governments gently suggest that the food industry take “voluntary steps to limit the marketing of unhealthy food options to children….” Did we just give up and give up control?
Our timid response to this obesity epidemic is combined with a national plan announced by the Joint Task Force of the American Society for Nutrition, the Institute of Food Technologists, and the International Food Information Council: the approach of “small changes.” Since “small changes are easy to make,” suggestions include “using mustard instead of mayonnaise” and “one meal instead of two donuts in the morning.” It seems like bringing a butter knife to a gun fight. Proponents of the minimal change approach complain that, unlike other drugs—for example, alcohol, cocaine, gambling, or tobacco—we cannot advise our obese patients to completely quit the habit, saying that “[n]o a person can stop eating.” But just because we have to breathe, it doesn’t mean that we have to pass the cigarette. And just because we have to eat doesn’t mean we have to eat junk food.
How about bringing a scalpel to a gunfight instead? The use of bariatric surgery has increased from approximately 40,000 procedures noted in the first international survey in 1998 to hundreds of thousands performed annually in the United States alone. The first method developed, intestinal bypass, involved severing up to 19 percent of the intestine. More than 30,000 intestinal bypass operations were performed before we saw the “catastrophe” and “catastrophic consequences” caused by these procedures. This included protein deficiency liver disease, “which often progresses to liver failure and death.” This terrible beginning is remembered as “one of the darkest spots in the history of surgery,” as I discuss in my video. Mortality Rate of Bariatric Surgery for Weight Loss.
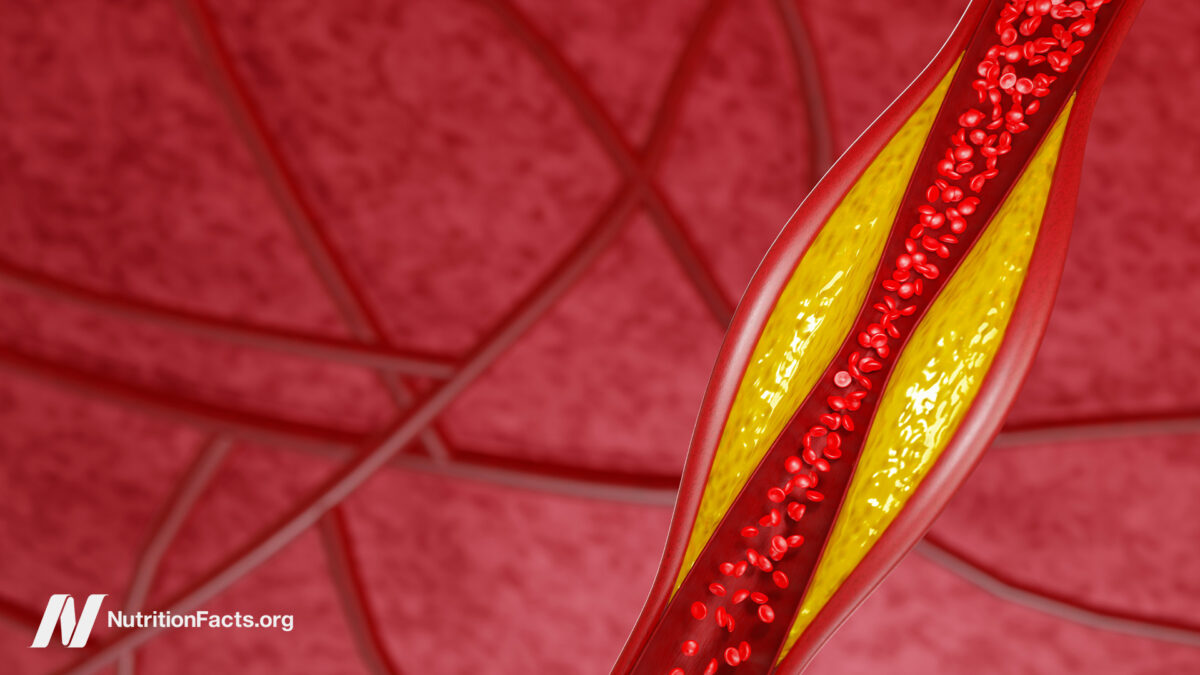
Today, death rates after bariatric surgery are considered “very low,” occurring on average in perhaps one in 300 to affect one in 500 patients. The most common procedure is a gastric bypass, also known as a sleeve gastrectomy, where most of the stomach is removed permanently. A small stomach tube is left to limit how much food people can eat at any given time. It’s surprising that many patients opt for bariatric surgery convinced that, “for them, ‘diet doesn’t work,'” when, in fact, that’s all the surgery can be—forced dieting. Bariatric surgery can be thought of as a type of internal jaw surgery.
Gastric bypass, also known as Roux-en-Y gastric bypass, is the second most common bariatric surgery. It includes obstruction—packing the stomach into a bag smaller than a golf ball—and malabsorption by reshaping the human body to bypass the first part of the small intestine. It appears to be more effective than simply cutting out a large portion of the stomach, resulting in a loss of up to 63% of excess weight compared to 53% of the gastric sleeve. But gastric bypass has a high risk of serious complications. Many are surprised to learn that “new surgical procedures…do not require market testing and approval by the Food and Drug Administration (FDA)” and are not exempt from strict regulatory scrutiny.
Doctor’s Note
I didn’t know there wasn’t some sort of approval process for new surgical procedures!
This is the first video in a four-part series about bariatric surgery. The following are:
My book How not to eat focuses only on sustainable weight loss. Check it out at your local public library or pick it up wherever you get your books. (All proceeds from my books are donated to charities.)